Fascia in MPS during cervical movement
Is the fascia involved in myofascial pain syndrome?
By Valentin C. Dones III, Ph.D.
Myofascial Pain Syndrome (MPS) is characterized by persistent pain in the shoulders and neck related to restricted neck movements, muscle weakness, and restricted functions (1). There are no significant differences in the prevalence of MPS between both sex; however, women exhibited greater pain sensitivity and disturbances in activities of daily living than men (2). Repetitive movements and prolonged static position predispose an individual to MPS. Acute MPS begins after traumatic events or overuse activities, where symptoms commonly resolve after a few weeks. But chronic MPS lasts six months or longer with widespread pain (3). It frequently involves the upper trapezius, enclosed by superficial and deep fasciae.
The clinical presentation of MPS is a limited neck movement, neck pain, tightness, or local twitch response in the shoulder and cervical region. Static posture and visual stress due to prolonged desk work form trigger points (4). The limited cervical movement was secondary to trigger points related to fascia adhesions causing movement restriction. Trigger points are the result of muscle overuse or damage, psychological stress from work-related duties, everyday heavy lifting, or continuous repetitive activity (1). Self-myofascial release, a physical therapy intervention, may restore fascia displacement in patients with musculoskeletal pain (5).
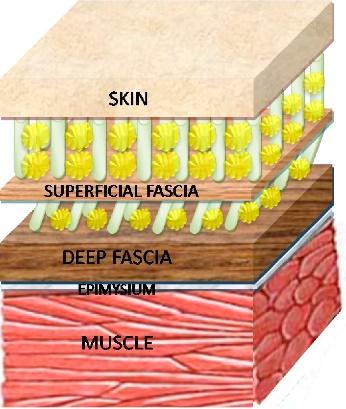
The superficial fascia and the deep fascia envelop the upper trapezius. Superficial fascia links the skin with the bone to the deep fascia (6). The structural link between the superficial fascia and muscle suggests that muscle contraction influences displacement of the superficial fascia. But the deep fascia is a multilayered structure formed by two to three layers of densely packed collagen fibers and a few scattered elastic fibers (7). Hyaluronan is found between the muscle’s deep fascia and within the muscle. Hyaluronan within the deep fascia would promote fascia displacement. The deep fascia covering the upper trapezius can possess adhesion points from repetitive strain injuries causing myofascial restrictions and dysfunctional movement patterns (8).
Reference. Stecco, C., Macchi, V., Porzionato, A., Duparc, F., & De Caro, R. (2011). The fascia: the forgotten structure. The Fascia: the Forgotten Structure, 127-138 (9).
Evidence for altered fascia displacement found in musculoskeletal conditions was reported in the literature. A case-control study said thoracolumbar fascia shear strain was 20% lower in participants with low back pain than participants without low back pain (10). But a cross-sectional study found a slight increase in linear fascia displacement in elbows with lateral epicondylalgia compared to elbows without lateral epicondylalgia (11).
In our investigation, we asked 300 participants with and without MPS to move their necks in six directions namely bending, looking up, left ear to left shoulder, right ear to right shoulder, looking to the right, and looking to the left. Our physiotherapist applied an overpressure at the end of the neck movement (Figure 2).

As the physiotherapy-sonographer, I scanned both shoulders of the participants while they were moving their necks (Figure 3). Using the Tracker by Brown and Christian (12), we measured the superficial and deep fascia displacements in over 3,350 ultrasound videos.

We found no differences in the superficial and deep fascia displacements between participants with and without MPS. There is no association between limited fascia displacements and MPS. We cannot use fascia displacements to differentiate individuals with MPS from those without MPS. Maybe other fascia abnormalities like fascia density are present in patients with MPS. Fascia density could be looked at besides how the fascia moves. The dense fascia can trap sensory nerve fibers, stop normal connective tissue movement, and reduce tissue extensibility, which can make it difficult for joints to move (13). Higher fascia density stops muscle spindles from shortening, which leads to chronic stretching, an increased stimulus to contract, and higher acetylcholine, which is linked to more myofascial pain (8).
Using myofascial release techniques and foam-rolling techniques on improving fascia mobility may be investigated in future studies. The difference in fascia displacement before and after therapy may explain the reported effectiveness of these interventions in reducing pain and improving neck movements of patients with MPS.
References
1. Jafri MS. Mechanisms of Myofascial Pain. Int Sch Res Not. 2014 Aug 18;2014:1–16.
2. Bourgaize S, Newton G, Kumbhare D, Srbely J. A comparison of the clinical manifestation and pathophysiology of myofascial pain syndrome and fibromyalgia: implications for differential diagnosis and management. J Can Chiropr Assoc. 2018 Apr;62(1):26–41.
4. Treaster D, Marras WS, Burr D, Sheedy JE, Hart D. Myofascial trigger point development from visual and postural stressors during computer work. J Electromyogr Kinesiol. 2006 Apr;16(2):115–24.
5. Kalichman L, Ben David C. Effect of self-myofascial release on myofascial pain, muscle flexibility, and strength: A narrative review. J Bodyw Mov Ther. 2017 Apr;21(2):446–51.
6. Blottner D, Huang Y, Trautmann G, Sun L. The fascia: Continuum linking bone and myofascial bag for global and local body movement control on Earth and in Space. A scoping review. REACH. 2019 Jun;14–15:100030.
7. McCOMBE D, Brown T, Slavin J, Morrison WA. The Histochemical Structure of the Deep Fascia and Its Structural Response to Surgery. J Hand Surg. 2001 Apr;26(2):89–97.
8. Stecco A, Gesi M, Stecco C, Stern R. Fascial Components of the Myofascial Pain Syndrome. Curr Pain Headache Rep. 2013 Aug;17(8):352.
9. Stecco C, Macchi V, Porzionato A, Duparc F, De Caro R. The fascia: the forgotten structure. Ital J Anat Embryol Arch Ital Anat Ed Embriologia. 2011;116(3):127–38.
10. Langevin HM, Fox JR, Koptiuch C, Badger GJ, Greenan- Naumann AC, Bouffard NA, et al. Reduced thoracolumbar fascia shear strain in human chronic low back pain. BMC Musculoskelet Disord. 2011 Dec;12(1):203.
11. Dones V, Suarez C, Rimando C, Yap M, Seril, Lopez J, et al. The use of Motion Tracking Analysis Program in detecting linear muscular displacement of the extensor digitorum communis in patients with Lateral Epicondylalgia: A cross-sectional study. Austin J Musculoskelet Disord. 2015;2(2):1021.
12. Brown D, Christian W. Tracker Video Analysis and Modeling Tool for Physics Education [Internet]. Tracker Video Analysis and Modeling Tool. 2021 [cited 2021 Aug 15]. Langevin HM, Sherman KJ. Pathophysiological model for chronic low back pain integrating connective tissue and nervous system mechanisms. Med Hypotheses. 2007 Jan;68(1):74–80.




